It's commonly assumed that machines "chase" large leaks by increasing pressure (if allowed) or keeping the pressure at the max (if you are already maxed out). That was apparently true of the older generations Auto machines. But the System One Auto algorithm will decrease the pressure when it detects a Large Leak in an attempt to help reseal the mask. (More about this later.)
Large Leaks in Encore.
Those of us using System Ones know all about how vague the whole issue of Large Leaks in Encore is. There's no numerical definition that is the equivalent of the RedLine in ResScan. Some people battle Large Leaks a lot of the time. Others hardly ever see an official Large Leak---even when they are leaking significantly. And the relationship between the expected leak rate for a given mask at a given pressure and the trigger for flagging something as a Large Leak also is murky and undocumented in the clinical and user manuals for our machines.
I've been using a PR System One BiPAP Auto now since 12/22/2010. That's 33 months. And in all that time, I've had exactly two Large Leaks flagged by Encore. I've had plenty of other (isolated) problems associated with leaking: The occasional dry mouth (or even wore, the mouth the tastes like something crawled in and died in it). The larger than normal bumps on the leak graph during particularly bad allergy nights or nights with serious congestion from the flu or a head cold. And numerous so-called "patient disconnects" where the machine mysteriously "loses" track of my breathing pattern, and the wave form peters out with smaller and smaller bumps until there's a gap in the wave form, but not the leak and pressure graphs. The "patient disconnects" also are earmarked by long series of PPs---I guess the machine is trying to use the PPs to sort out the breathing pattern. Many of these occasional leak problems occur when my total leak rate is around 20-25 L/min above my expected leak rate---in other words, these occasional problems occur when my leak rate would likely lie near or above the RedLine in ResScan. But as I've said, Encore has only flagged one Large Leak in the 21 months I've used the machine.
My first official Large Leak has a number of features in it that may be useful to look at as a way of helping others understand just what can go on during an official Large Leak as well as illustrate why leaks that are large, but not large enough to be officially flagged as Large Leaks may also be problematic---both in terms of quality of therapy and in terms of accuracy of the data.
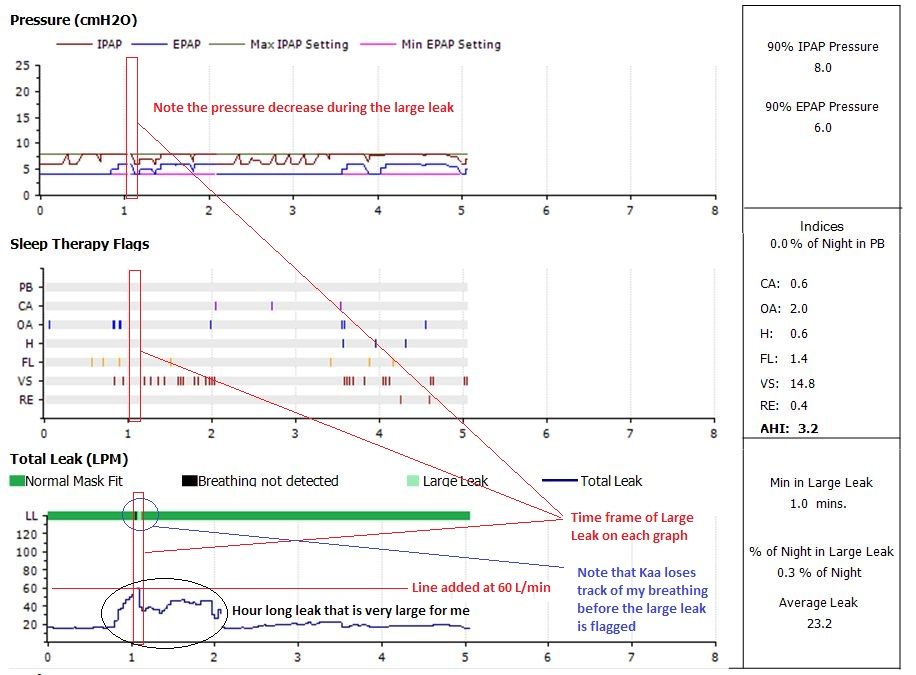
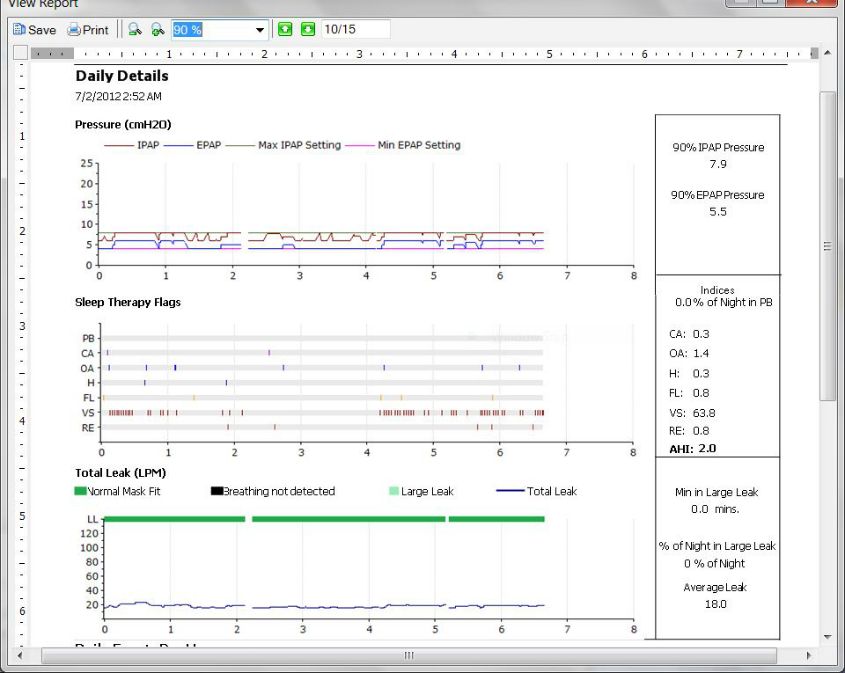
Here's the full night's data as shown in Encore:
The one minute long Large Leak, of course, is flagged by the light green bar in the leak graph. One thing that I want to point out is that during the Large Leak, my machine (Kaa) decreases the pressure rather than increases it. It's commonly assumed that machines "chase" large leaks by increasing pressure (if allowed) or keeping the pressure at the max (if you are already maxed out). That was apparently true of the older generations Auto machines. But the System One Auto algorithm will decrease the pressure when it detects a Large Leak in an attempt to help reseal the mask. (More about this later.)
I's also worth pointing out the ugly Black bar in the leak graph that immediately precedes the light green "Large Leak" indicator. Black bars like this in Encore leak lines mean that the machine was ON, but it could not detect a meaningful breathing pattern. If you take the mask off and leave the machine running, you'll get one of these big ugly Black Bars. But in the presence of Large Leaks, the machine can have trouble detecting the breathing pattern and ear mark the period in Encore with an ugly Black Bar. Also note the small breaks in the pressure line and the leak graph that correspond to that Black Bar of "no breathing detected". As we'll see in a minute, that seems to be an artifact of Encore.
The same Large Leak in SleepyHead
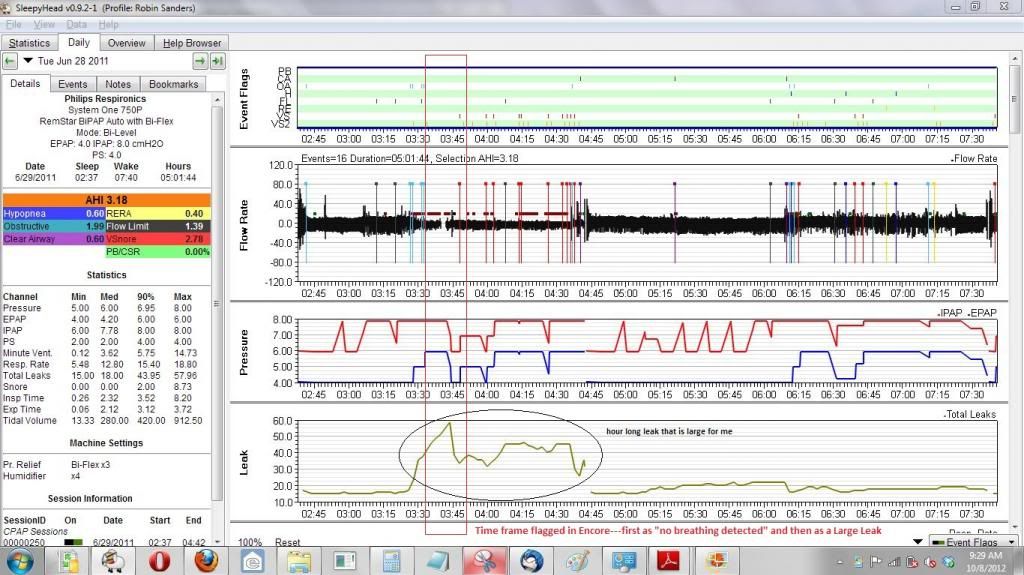
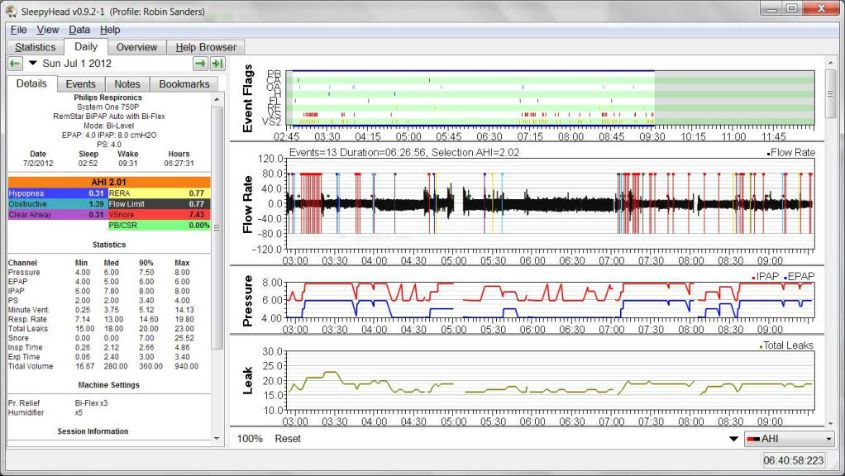
Here's the same night's data viewed in SleepyHead:
Note that SleepyHead has no way of flagging an "official Large Leak" in the data. In looking at lots of data from forum members on cpaptalk.com, it seems safe to say that Encore's Large Leak flags depend on both the pressure and on whether the System One is a Series 50 or a Series 60 machine.
In SleepyHead, we see a break in the wave form (where the Black Bar over the leak graph is in Encore) preceding the biggest bump on the Leak graph. For those who track such things---SleepyHead says that the maximum leak rate topped out at 57.96 L/min, which is about three times my usual, expected leak rate of 18-20 L/min (based on many many nights of SleepyHead data) and about twice my mask's published expect leak rate of 29 L/min at my maximum pressure of 8cm. (Note, however, that my leak rates seem to follow the leak rate numbers of my EPAP, which ranges from 4 to 6 rather than my IPAP.)
Also of note are all those little Pressure Pulse (PP) boxes sprinkled throughout the hour-long leak that is both abnormally long and abnormally large for me. More on these clusters of PPs in a bit.
What actually happens during the Large Leak?
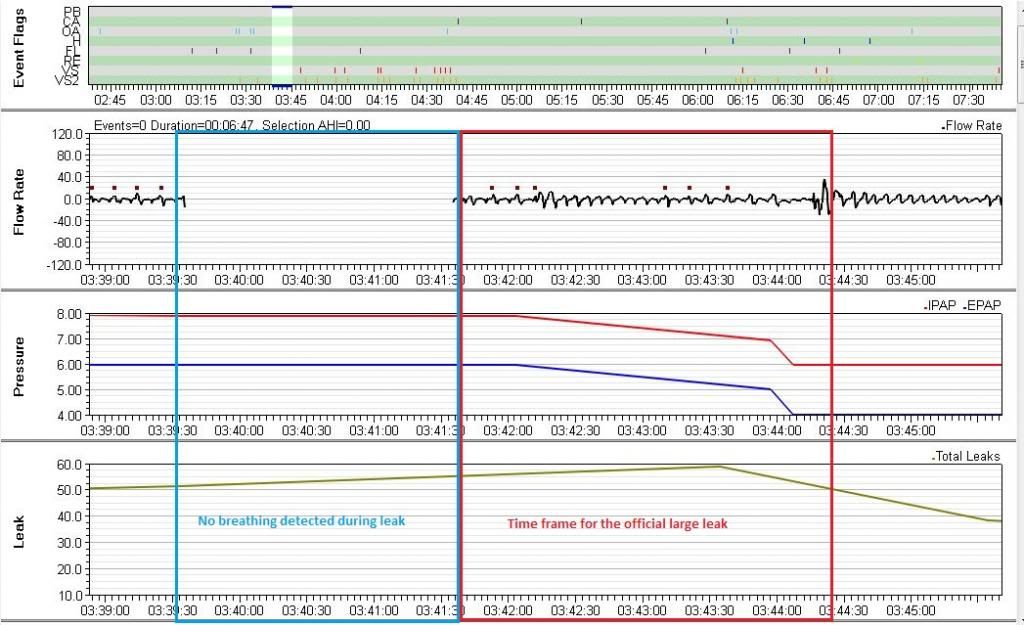
Let's zoom in on the period right around where Encore puts the big Black Bar and the Large Leak is flagged. This is what we see in SleepyHead when we focus right our attention on the Large Leak itself:
This close up shows that Sleepy Head definitely has no break in the pressure and leak graphs at the Large Leak, the way the Encore graphs did.
Now note how the wave form is severely compressed near the 0 line just before and just after the gap in the wave flow. This indicates that Kaa could not reliably determine whether there was much air going into or out of my lungs. Note how when the wave form picks up after the gap, it's still pathetic looking. And also note that it has none of the characteristics of what my wave form usually like when I'm awake enough to turn Kaa off and back on. So I'm fully asleep during this part of the leak.
And notice all those PPs right before the gap in the wave form and right after the wave form picks back up? I believe those PPs are being used by Kaa to try to figure out if there's a live, breathing person at the other end of the hose. I think Kaa realizes that these periods of very low variation in the wave flow are way too long to be a typical apnea or hypopnea, and that's why they are not flagged as such. But it also gets so befuddled about what it's seeing in the wave form data, that Kaa concludes I must not be breathing through the mask and it drops the wave form recording all together during the time it cannot determine any meaningful breathing pattern--and the period of "no detectable breathing" is earmarked by the ugly Black Bar in Encore. When I showed my DME this wave form pattern (in a different context), the RT referred to it as a "patient disconnect". (And yes, that bothered me because "patient disconnect" seems to imply that I, the patient, disconnected the machine from my nose. And I most certainly did NOT do that here or anywhere else where I've seen these patient disconnects.) So from now on, I'll call those wave patterns "patient disconnects" even though I don't like that language at all.
A couple of minutes after Kaa detects the "patient disconnect" Kaa finds rudimentary evidence of breathing again, so it starts recording the wave form data. But by this point the leak rate has also grown to about 55 L/min and Encore (and Kaa) decide to flag this as a Large Leak. As in---there's breathing present and the leak is now large enough to meet that unknown standard of Large Leak. And it's important to note that almost as soon as the Large Leak is detected, Kaa starts to lower my pressures: First from 8/6 to 7/5 and then more sharply from 7/5 to 6/4. Kaa is attempting to help limit or even fix that Large Leak by lowering the pressures---exactly as the description of the PR Auto algorithm says it is supposed to do in the presence of Large Leaks.
As far as accuracy of recording events during this Large Leak: Because Kaa can barely detect a breathing pattern, it's clear that the usual definitions used to flag OAs, CAs, and Hs are going to be difficult to apply: They all rely on a reasonably accurate baseline of the current airflow into/out of the lungs and that baseline is calculated using several minutes worth of data. Because the breathing pattern is barely there, it's almost impossible for the machine to detect enough of a decrease in airflow to trigger flagging an OA or a CA or an H throughout the Large Leak (and even in the part of the longer, not-quite-so-large leaks immediately preceding and following the official Large Leak itself. And hence there's no good reason to believe that this time frame is really as "event-free" as the event chart makes it appear to be.
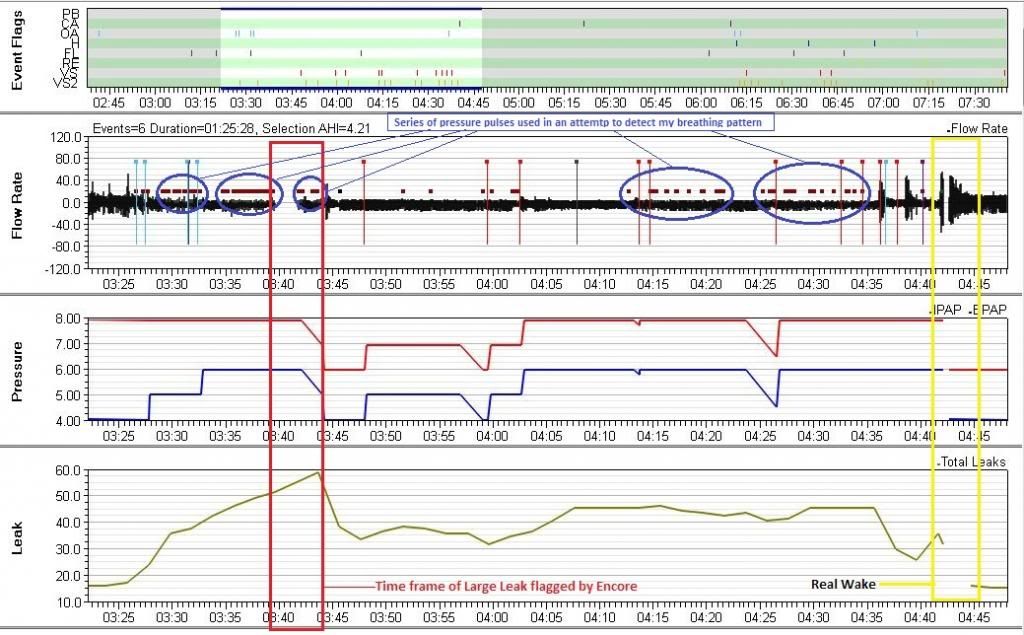
Now I want to zoom out just a bit---to see the entire hour of leaking that was large by my data's usual numbers, but not large enough to be flagged as a Large Leak in Encore. Here's a picture of the whole hour-long leak:
Those pesky PP boxes that pop up throughout this hour long period correlate closely to the periods of highest leak rates during this leaky hour---but most of those leaks are NOT large enough to be flagged by Encore as Large Leaks. And when I zoom in on those clusters of PPs, the wave forms look almost as anemic and as squashed as the wave form during the close up of the large leak. In other words, it's clear from the PPs and wave form that Kaa was having trouble tracking my breathing for much of this leaky hour---not just the part flagged as a Large Leak by Encore. In other words, when the leak rate is flirting with Large Leak territory, the machine can have a tough time sorting out what's actually going on in the wave form. And that clearly means that data during periods with "patient disconnects" and wave flow patterns associated with "patient disconnects" may not be very accurate: You can't detect an apnea or hypopnea if you can't detect the breathing pattern in the first place.
It's also clear at this level of magnification that the gap in the wave form during the Large Leak (the "patient disconnect") is distinctly different from the gap in the wave form where I wake up and turn the machine off and then back on.
What might have caused this Large Leak? And how did it affect the quality of my sleep?
Well there's a pair of "double" OA's that occur right around 3:30---one pair occurs a bit before 3:30 and the other occurs a bit after. Each pair of OA's causes my EPAP to increase by 1cm. My IPAP was already running at 8cm due to some earlier flow limitations and the hunt-and-peck part of the PR Auto algorithm. I seriously doubt the 2cm increase in EPAP lead to the leak. It's not an uncommon event in my data and 8/6 is still relatively low pressure. My guess is that about the time of that pressure increase I started mouth breathing. Mouth breathing is a rare thing for me, but we were in NJ in late June 2012 on this night, and that's peak allergy season for me. And there's a lot of snoring going on during that leak. I usually snore with my mouth closed, but in allergy season? Open mouth snoring does occasionally happen to me. But I could also have dislodged one of the nasal pillows somehow. Or perhaps one of the pillows became inverted. Or maybe it was a combination of all these things.
But what ever happened, the leak continued to grow until the machine lost track of my breathing and the leak was large enough to trigger a Large Leak flag. I still didn't wake up (which rather amazes me), but once the machine lowered the pressure back down to 6/4, the peak of the large leak rate decreased. Possibly my mouth partly closed. Possibly the dislodged nasal pillow was partially able to reseat itself. Whatever. But leaking remained an issue---either I kept breathing through my mouth or that pesky pillow remained out of place. And as the pressures fluctuated (mainly due to SNORING), so did the leak---never as far into Large Leak territory as the beginning of the leak, but high enough up where the machine was worried about whether it was tracking breathing or not. And while the machine was able to detect SNORING, it certainly was not detecting anything that met its definitions of OAs or Hs, possibly because the wave flow itself was so difficult to detect at all when the leak as high as 45 L/min.
By 4:45 I'm clearly restless: There's a possible snoring arousal followed by an OA (that may be due to transitioning back to sleep) followed by more snoring, another possible arousal and a CA (that may be transitional) and the real wake where I am conscious enough to turn Kaa off and back on and in the process fix whatever the problem that caused the leak was. Certainly if it was mouth breathing, I didn't open my mouth again for the rest of the night. Or perhaps it was that I did find and fix the dislodged nasal pillow at the wake. My sleep log notes a couple of wakes and lots of aerophagia and a general lousy feeling in the morning after this night. So this leak, together with the higher than normal AHI for the rest of the night as well did disturb my sleep.
Fortunately, this kind of leaking is pretty rare for me. This particular hour long leak is both larger and longer than even the worst of my "typical" leaks. The worst of my leaks typically top out around 40 or 45 L/min and I don't have many of them that large. My bad leaks are typically less than 30 minutes in length, with a few of them lasting as long as this one. I typically see a 30-40 minute "bad" leak maybe two or three times a month at most. But they often have multiple PPs in them without events being flagged and they occasionally have "patient disconnects" in them as well. But note that I have also had "patient disconnects" where there was no leaking going on. And because this kind of a large leak is such a rare occurrence in my data, I'm comfortable to writing it off as a visit from the aliens. But if I were seeing this kind of leaking going on several times a week (instead of a few times a month), I'd be inclined to work on figuring out what was causing the problems.